What You Need to Know About COVID-19
Visit the CDC for the most up-to-date information on COVID-19.
For more information, please visit:
Coronavirus disease (COVID-19) was identified in 2019 as an emerging illness. In the past few years, we've gained a great deal of knowledge about treatment options, how the virus works, and the total impact of the illness. New information, obtained daily, will further inform the risk assessment, treatment options and next steps.
About COVID-19
- What is COVID-19?
COVID-19 is a disease that affects breathing. It's caused by a virus called a coronavirus, which can spread from person to person. People of all ages can get infected. Older adults and people with pre-existing medical conditions may be more likely to become gravely ill if infected. - What are the symptoms?
The symptoms of coronavirus include mild to severe respiratory symptoms. Symptoms include fever, cough, and shortness of breath, and lower respiratory illness. COVID-19 can be contagious before a person begins showing symptoms - What else causes similar symptoms?
Influenza (the flu), a contagious respiratory illness caused by the influenza viruses (Type A and Type B), has high activity in the United States at this time. Everyone 6 months of age and older should get a flu vaccine. Contact your PCP to get a flu vaccine.
Prevention and Screening
Protect yourself and your community
We all have a role to play in protecting our communities and families from the spread of coronavirus. It is similar to other communicable viruses. You can also follow these tips to prevent infection:
- Stay up to date with all vaccines including COVID-19 and flu.
- Wash your hands thoroughly and frequently. Use soap and water for at least 20 seconds.
- Use an alcohol-based hand-sanitizing rub (must contain at least 60 percent alcohol).
- Cover your mouth when you cough or sneeze by coughing/sneezing into your elbow.
- Promptly dispose of tissues in a wastebasket after use.
- Clean public surfaces thoroughly.
- Stay home when you are sick.
- Avoid shaking hands.
- Avoid close contact with people who are sick.
Check CDC COVID-19 Community Level tool for prevention steps based on your county.
What is the COVID-19 Vaccine?
A COVID-19 vaccine helps give you the best chance of keeping yourself and your loved ones safe from getting COVID-19 symptoms. And, the vaccine will help keep you from getting COVID-linked health problems in the future.
There are several COVID-19 vaccines that have been fully approved by the FDA.
For more information on COVID-19 vaccines, including safety, doses, boosters and more, see the CDC vaccine guidelines for the most current information.
You can also find vaccine information from the Advisory Committee on Immunization Practices (ACIP).
Lane County
Lane County COVID-19 Vaccine Clinics
Where can I get the COVID-19 vaccine?
To find out if you are eligible to receive the COVID-19 vaccine, you can text message ORCOVID to 898211 for a quick reply. You can also visit Get Vaccinated Oregon to find out if you are eligible and for next steps. You may also contact your doctor or pharmacist with questions about when and how you may receive the vaccine.
Local public health agencies and health care systems are working on vaccine distribution. Find vaccine distribution information on the Oregon Health Authority website.
Lane County Pre-Registration
- COVID-19 Vaccine Pre-Registration Form – English
- COVID-19 Vaccine Pre-Registration Form – En Español (Spanish)
If you are unable to access the Internet, you may call the LCPHA (Lane County Public Health Authority) Call Center at 541-682-1380.
Tri-Counties
Tri-Counties Pre-Registration
All Oregonians, including senior adults age 65 and over, can sign up to be notified about vaccination events when they are eligible at Get Vaccinated Oregon using the signup tool.
The new appointment scheduling process for eligible older adults who live in Clackamas, Columbia, Multnomah or Washington counties will be based on names being pulled from the Get Vaccinated Oregon tool.
Do I have to pay for my vaccine? Or get prior authorization?
No. Both doses of the COVID-19 vaccine will be at no cost to you. You do not need to get a prior authorization for your vaccine. Note: This is subject to change at any time per Division of Financial Regulation (DFR).
At-Home COVID-19 Tests
How do I get an at-home COVID-19 test for free?
No Cost At-Home Tests Through June 30, 2023
If you have pharmacy coverage as part of your Health Net Health Plan of Oregon, Inc. (Health Net) plan, you can get an over the counter (OTC), FDA-approved, EUA at-home COVID-19 test at no cost if you visit one of Health Net's in-network retail pharmacies. View approved in-network pharmacy test kit list (PDF).
Get the test from the pharmacy itself. Do not get a test and pay for it at the store's normal register. If you pay for the test at the normal register, then you will need to submit a medical claim form to get reimbursed.
Visit our website to find an in-network pharmacy for your plan type.
Beginning July 1, 2023, At-Home COVID-19 Tests will not be covered.
Are there tests not covered through pharmacy?
COVID test kits that are not covered include:
- Kits that have to be sent to a lab (collection kits)
- Kits that are not indicated as "OTC"
- COVID kits obtained outside of the United States
Beginning July 1, 2023, At-Home COVID-19 Tests will not be covered.
I have a Health Net group medical plan, but the prescription coverage is through another company. How do I get an at-home COVID test for free?
Check with your prescription plan company to see if you can get an OTC at-home COVID-19 test at no cost.
Through June 30, 2023, you can purchase an OTC FDA- approved, EUA at-home COVID-19 test and be reimbursed by Health Net for the cost of the test. Please complete and submit a Health Net medical claim form. Beginning July 1, 2023, At-Home COVID-19 Tests through Health Net will not be covered.
I bought an at-home COVID-19 test on my own, will I be reimbursed?
Through June 30, 2023
Yes. If you bought an OTC FDA-approved, EUA at-home COVID-19 test at any place outside of our in-network pharmacies (e.g., Amazon, grocery store, drug store, etc.), you will be reimbursed for the cost of the test kits (up to $12 per test) as follows:
- Purchase an at-home test that is on the FDA-approved EUA list. View the FDA-approved EUA at-home test list. Tests available without a prescription will include "OTC" (for over-the-counter at-home tests) in the Attributes column.
- Complete and submit a separate claim form for each member:
- You must include a copy of your receipt. On your receipt, write or circle (if the information is on the receipt):
- The name of the OTC COVID Test Kit.
- The UPC code found on the box.
- Complete Section 1 and Section 2 of the claim form.
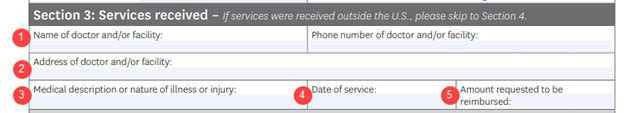
- For Section 3, include this information in the fields as follows:
- The store where you bought the test kit (Amazon, grocery store name, drug store name, etc.)
- The address of the store if applicable.
- Write "COVID-19 Home Test" and the number of tests.
- The date you purchased the kit(s).
- The amount being asked for reimbursement.
- Sign and return your claim form (don't forget the receipt).
Mail to: Health Net Health Plan of Oregon, Inc.
PO Box 9040
Farmington, MO 63640-9040 - You will be reimbursed based on federal guidance set on January 10, 2022 which states:
- The cost of the at-home test – up to $12 per test
- Maximum of 8 tests per covered member in a 30-day period
- A single testing kit box that includes two tests would count as two (e.g. $12 x 2 = $24)
If you purchased a physician ordered, FDA/EUA approved test before January 15, 2022, Health Net will reimburse you when the claim form is turned in based on what you paid.
Beginning July 1, 2023, At-Home COVID-19 Tests will not be covered.
If I bought an FDA-approved EUA at-home COVID-19 test on Amazon, how do I show my proof of purchase?
Please print an image of the digital receipt and submit it along with the claim form. If you can't provide a digital receipt, please put the order or invoice number for the purchase on the claim form. This is for proof of purchase and tracking. See above FAQ on how to be reimbursed.
Will Health Net limit the number of tests that a member can get for free?
Yes. Health Net will cover 8 OTC FDA-approved, EUA at-home COVID-19 tests purchased over-the-counter per covered member in a 30-day period. This follows the federal guidance released on January 10, 2022.
Beginning July 1, 2023, At-Home COVID-19 Tests will not be covered.
Insurance and Cost
Does my Health Net plan cover COVID-19 testing/screening?
Through June 30, 2023
When medically necessary diagnostic testing, or medical screening services is ordered and/or referred by a licensed health care provider, we will cover the cost of medically necessary COVID-19 tests and screenings. If applicable, your plan's copayment, coinsurance and/or deductible cost-sharing requirements will be waived for medically necessary COVID-19 diagnostic testing and medical screening services.
Beginning July 1, 2023
COVID-19 PCR testing/screening ordered through an in-network provider will follow the plan's benefits. A cost-share will apply. Out-of-network coverage/limits will be based on your plan.
Does my Health Net plan cover COVID-19 treatment services?
COVID-19 treatment is a covered benefit. Cost-share applies based on certain services. See your Plan Coverage Document.
Is prior authorization required for COVID-19 testing, screening services and/or treatment under my Health Net plan coverage?
Our Health Net plans will not require prior authorization, prior certification, prior notification and/or step therapy protocols for medically necessary COVID-19 diagnostic testing and medical screening services when medically necessary services are ordered and/or referred by a licensed health care provider. Effective July 1, 2021, prior authorization requirements for COVID-19 treatment and virtual care are required.
